Discover what Emgality® can do for patients with episodic migraine1

For your patients with 4 to 14 MHDs per month1
Emgality delivered significantly more migraine-free days vs placebo1
Emgality prevented significantly more mean monthly MHDs vs placebo1a:
- EVOLVE-1: 4.7 with Emgality 120 mg (N=210) vs 2.8 with placebo (N=425) (baseline mean: 9.2 vs 9.1) over Months 1 to 6 (p<0.001)
- EVOLVE-2: 4.3 with Emgality 120 mg (N=226) vs 2.3 with placebo (N=450) (baseline mean: 9.1 vs 9.2) over Months 1 to 6 (p<0.001)
Emgality reduced mean monthly MHDs1
Mean Change From Baseline in Monthly MHDs1,2a
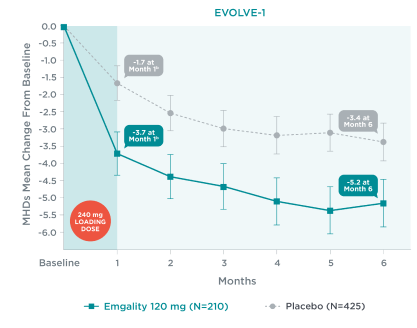

aLS means and 95% confidence intervals are presented.1,2,4
bEarliest post-baseline, prespecified assessment.
EVOLVE-1
Mean change from baseline in monthly MHDs at each month over Months 1 to 6 in EVOLVE-11,2a:
- Month 1: Emgality following the loading dose of 240 mg was -3.7b vs - 1.7b for placebo
- Month 2: Emgality 120 mg was -4.4 vs -2.5 for placebo
- Month 3: Emgality 120 mg was -4.7 vs -3.0 for placebo
- Month 4: Emgality 120 mg was -5.1 vs -3.2 for placebo
- Month 5: Emgality 120 mg was -5.4 vs -3.1 for placebo
- Month 6: Emgality 120 mg was -5.2 vs -3.4 for placebo
210 patients were treated with Emgality 120 mg vs 425 patients treated with placebo.
EVOLVE-2
Mean change from baseline in monthly MHDs at each month over Months 1 to 6 in EVOLVE-21,2a:
- Month 1: Emgality following the loading dose of 240 mg was -3.9b vs - 1.2b for placebo
- Month 2: Emgality 120 mg was -4.0 vs -2.2 for placebo
- Month 3: Emgality 120 mg was -3.8 vs -2.2 for placebo
- Month 4: Emgality 120 mg was -4.5 vs -2.4 for placebo
- Month 5: Emgality 120 mg was -4.9 vs -2.9 for placebo
- Month 6: Emgality 120 mg was -4.6 vs -2.9 for placebo
226 patients were treated with Emgality 120 mg vs 450 patients treated with placebo.
No formal hypothesis testing was conducted to evaluate treatment difference in mean monthly MHD reduction at each month. However, patients treated with Emgality 120 mg showed a nominally greater reduction in number of monthly MHDs at each month compared to placebo.1,2
See MHD data for chronic migraine.
See study design for EVOLVE-1 and EVOLVE-2.
SELECT IMPORTANT SAFETY INFORMATION
Contraindications
Emgality is contraindicated in patients with serious hypersensitivity to galcanezumab-gnlm or to any of the excipients.
For your patients with 4 to 14 MHDs per month1
Emgality is the first and only CGRP antagonist antibody that evaluated and demonstrated significance vs placebo in 100% response rates in two phase 3 trials1,5-9
Mean Percentage of Patients Meeting Defined Levels of Reduction in Monthly MHDs Over Months 1 to 61
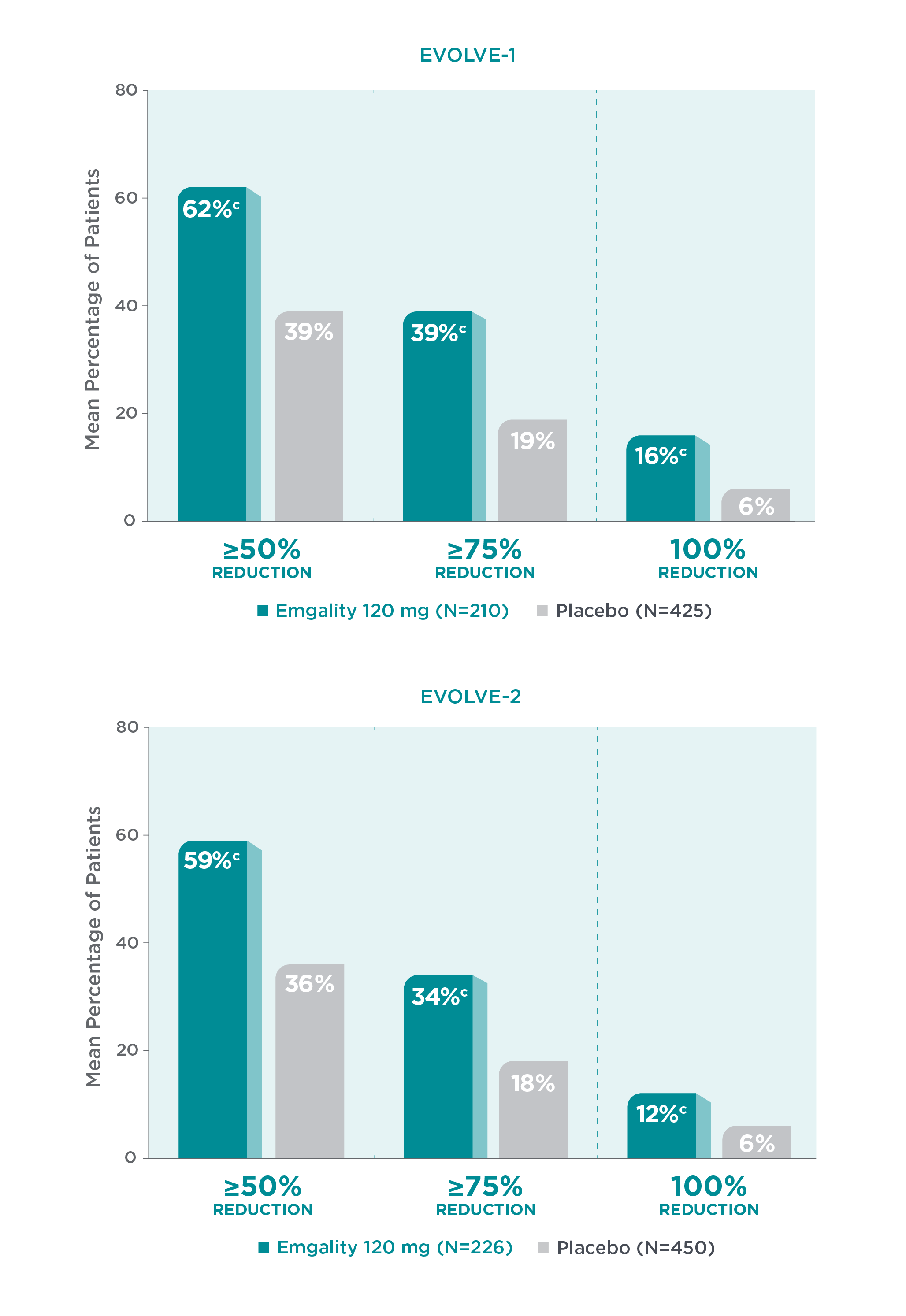
cp<0.001 vs placebo.1
CGRP=calcitonin gene-related peptide; LS=least-square; MHD=migraine headache day.
EVOLVE-1
Response rates defined levels of reduction in monthly MHDs over Months 1 to 6 in EVOLVE-11:
- Mean percentage of patients who experienced a ≥50% reduction in MHDs with Emgality 120 mg was 62%c vs 39% with placebo respectively
- Mean percentage of patients who experienced a ≥75% reduction in MHDs with Emgality 120 mg was 39%c vs 19% with placebo respectively
- Mean percentage of patients who experienced a 100% reduction in any month of the 6-month study was 16%c with Emgality vs 6% with placebo respectively
210 patients were treated with Emgality and 425 patients were treated with placebo.
EVOLVE-2
Response rates defined levels of reduction in monthly MHDs over Months 1 to 6 in EVOLVE-21:
- Mean percentage of patients who experienced a ≥50% reduction in MHDs with Emgality 120 mg was 59%c vs 36% with placebo respectively
- Mean percentage of patients who experienced a ≥75% reduction in MHDs with Emgality 120 mg was 34%c vs 18% with placebo respectively
- Mean percentage of patients who experienced a 100% reduction in any month of the 6-month study was 12%c with Emgality vs 6% with placebo respectively
226 patients were treated with Emgality and 450 patients were treated with placebo.
In REGAIN, Emgality 120 mg was not significantly better than placebo for the mean percentage of patients with ≥75% or 100% reduction from baseline in the number of monthly MHDs over the 3-month treatment period.1
See MHD response rate data for chronic migraine.
SELECT IMPORTANT SAFETY INFORMATION
Hypersensitivity Reactions
Hypersensitivity reactions, including dyspnea, urticaria, and rash, have occurred with Emgality in clinical studies and the postmarketing setting. Cases of anaphylaxis and angioedema have also been reported in the postmarketing setting. If a serious or severe hypersensitivity reaction occurs, discontinue administration of Emgality and initiate appropriate therapy. Hypersensitivity reactions can occur days after administration and may be prolonged.
References
- Emgality. Prescribing Information. Lilly USA, LLC.
- Data on File. Lilly USA, LLC. DOF-GZ-US-0002.
- Mulleners WM, Kim BK, Láinez MJA, et al. Safety and efficacy of galcanezumab in patients for whom previous migraine preventive medication from two to four categories had failed (CONQUER): a multicentre, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 2020;19(10):814-825.
- Data on File. Lilly USA, LLC. DOF-GZ-US-0120.
- Stauffer VL, Dodick DW, Zhang Q, et al. Evaluation of galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurol. 2018;75(9):1080-1088.
- Skljarevski V, Matharu M, Millen BA, et al. Efficacy and safety of galcanezumab for the prevention of episodic migraine: results of the EVOLVE-2 Phase 3 randomized controlled clinical trial. Cephalalgia. 2018;38(8):1442-1454.
- Aimovig. Prescribing Information. Amgen Inc.
- Ajovy. Prescribing Information. Teva Pharmaceuticals USA, Inc.
- Vyepti. Prescribing Information. Lundbeck Seattle BioPharmaceuticals, Inc.